I live with multiple autoimmune disorders, including Celiac Disease and the lesser understood Sjogren's Syndrome. I also have a neurospicy combo of ADHD, Bipolar Disorder, and PTSD, so I'm really a vision of pristine health. 
I mention the mental health stuff only because of the intersection of symptoms and the ways in which my physical and mental health can play off of each other when it comes to flares and episodes.
But! I'm here to talk about the autoimmune stuff.
Both of these disorders are lifelong diagnoses, and there is currently no cure for either. Sjogren’s has the potential to progress to more severe symptoms with age. They are very exhausting to manage, and finding the right care team is critical.
Anyway, AMA!
I mention the mental health stuff only because of the intersection of symptoms and the ways in which my physical and mental health can play off of each other when it comes to flares and episodes.
But! I'm here to talk about the autoimmune stuff.
About Celiac Disease
Celiac Disease is an autoimmune disorder in which the consumption of gluten (found in certain grains that are common in many foods) causes the body to have an immune response and attack healthy tissue. This is distinctly different from gluten sensitivity or intolerance which cause gastrointestinal distress.
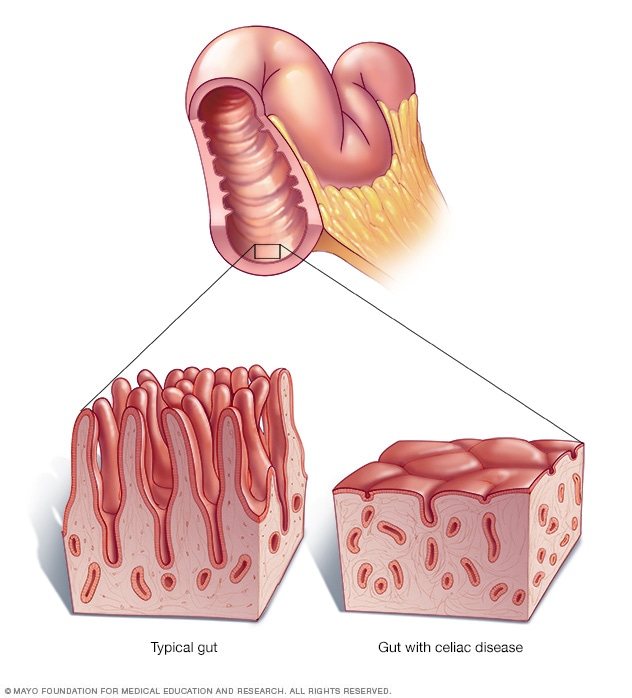
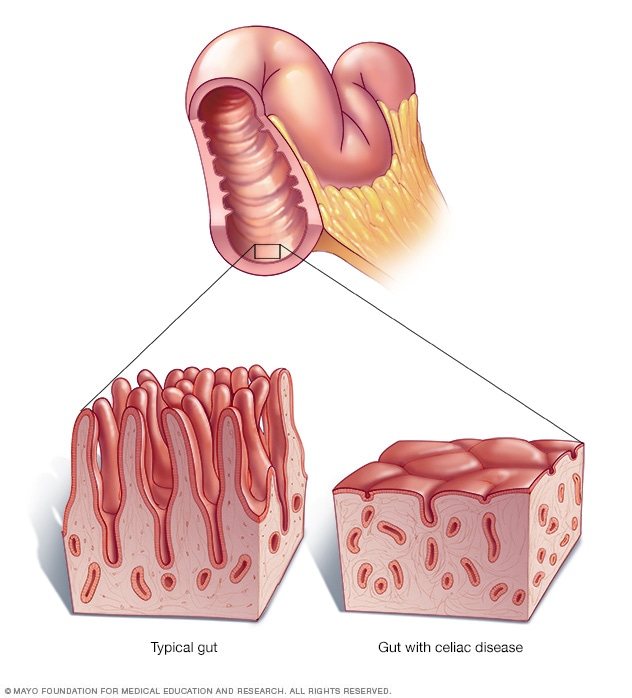
Your small intestine is lined with tiny hairlike projections called villi, which absorb sugars, fats, proteins, vitamins, minerals and other nutrients from the food you eat. Gluten exposure in people with celiac disease damages the villi, making it hard for the body to absorb nutrients necessary for health and growth.
As you can imagine, not being able to absorb nutrients properly can lead to systemic problems beyond what often gets misdiagnosed as Irritable Bowel Syndrome (IBS). In my case, at various points in my life, I’ve also suffered from stunted growth, mouth ulcers (“canker sores”), stomach ulcers, gastroesophageal reflux disorder (GERD), low bone density, loss of tooth enamel, pelvic pain, and reproductive issues so severe that they nearly required a hysterectomy in my 20s (thankfully resolved without major surgery).
Additionally, I am intolerant to the entire onion family (including garlic *sob*), fructose, legumes, lactose, artificial sweeteners/sugar alcohols, and peppers.
(Some of my friends playfully refer to me as “the food-intolerant hussy.”)
I was finally diagnosed with Celiac in 2020 at the age of 32, but my history of symptoms was lifelong, and my journey to diagnosis began in 2012 with a visit to a gastroenterologist to help pinpoint why I was sick every single day.
The good news is that eliminating gluten from my diet has not only made me feel better, but has allowed certain symptoms and damage to heal. This condition is controlled primarily with a strict diet and does not need medication to address primary symptoms.
Celiac Disease is an autoimmune disorder in which the consumption of gluten (found in certain grains that are common in many foods) causes the body to have an immune response and attack healthy tissue. This is distinctly different from gluten sensitivity or intolerance which cause gastrointestinal distress.
Your small intestine is lined with tiny hairlike projections called villi, which absorb sugars, fats, proteins, vitamins, minerals and other nutrients from the food you eat. Gluten exposure in people with celiac disease damages the villi, making it hard for the body to absorb nutrients necessary for health and growth.
TW: medical diagram of villi
As you can imagine, not being able to absorb nutrients properly can lead to systemic problems beyond what often gets misdiagnosed as Irritable Bowel Syndrome (IBS). In my case, at various points in my life, I’ve also suffered from stunted growth, mouth ulcers (“canker sores”), stomach ulcers, gastroesophageal reflux disorder (GERD), low bone density, loss of tooth enamel, pelvic pain, and reproductive issues so severe that they nearly required a hysterectomy in my 20s (thankfully resolved without major surgery).
Additionally, I am intolerant to the entire onion family (including garlic *sob*), fructose, legumes, lactose, artificial sweeteners/sugar alcohols, and peppers.
(Some of my friends playfully refer to me as “the food-intolerant hussy.”)
I was finally diagnosed with Celiac in 2020 at the age of 32, but my history of symptoms was lifelong, and my journey to diagnosis began in 2012 with a visit to a gastroenterologist to help pinpoint why I was sick every single day.
The good news is that eliminating gluten from my diet has not only made me feel better, but has allowed certain symptoms and damage to heal. This condition is controlled primarily with a strict diet and does not need medication to address primary symptoms.
About Sjogren’s Syndrome
Sjogren’s Syndrome (SS) is a Rheumatoid Autoimmune Disease, in the same category as the more well known illness Rheumatoid Arthritis, as well as Lupus (and a couple hundred more). Because of this, people with Sjogren’s are at risk for developing additional rheumatoid disorders in the future (RA runs in my family, RIP me).
The primary symptoms of SS manifest as pervasive dryness of the eyes, mouth, throat, and sinuses (as well as certain reproductive anatomy in some AFAB patients). This is because the autoimmune response triggered by SS causes the body to produce less saliva, tears, and fluid in the aforementioned reproductive anatomy.
Unfortunately, these symptoms have a lot of comorbidity with other conditions, and so it’s very commonly misdiagnosed and underdiagnosed.
SS can also cause systemic issues. In my case, I often experience breathing difficulties at night caused by my dry sinuses (which are partially calcified) and the thickening of mucus in my throat. Additionally, I suffer from full body joint and nerve pain flares, fatigue flares, tooth decay (bacteria growth exacerbated by dry mouth), and brain fog and memory loss. SS can also potentially affect the function of vital organs and the gastrointestinal tract.
Unlike my Celiac disease, which can be controlled simply by eliminating gluten from my diet, my SS is managed with several medications that I must take daily (some throughout the day). I juggle a rheumatologist, an optometrist, a neuro-ophthalmologist, a dentist, an oral surgeon, and my primary care provider for the management of this disease. (On top of providers I see for other conditions.)
My Sjogren’s was diagnosed last year almost by happenstance in the course of trying to address pervasive double vision, which led to us discovering I had very dry eyes and an inflamed optic nerve, which led to me getting an MRI, which found a benign brain tumor, which led to me seeing a very knowledgeable neurologist who gave me a blood test for Sjogren’s related antibodies on a hunch and bam! I got my diagnosis and a referral to a rheumatologist. This is ironically a much more straightforward path to diagnosis than most SS patients experience and only took about three months.
(Sjogren’s had nothing to do with the double vision, which turned out to be muscular and fixable with prism glasses. Figuring out the inflamed optic nerve is ongoing.)
Sjogren’s Syndrome (SS) is a Rheumatoid Autoimmune Disease, in the same category as the more well known illness Rheumatoid Arthritis, as well as Lupus (and a couple hundred more). Because of this, people with Sjogren’s are at risk for developing additional rheumatoid disorders in the future (RA runs in my family, RIP me).
The primary symptoms of SS manifest as pervasive dryness of the eyes, mouth, throat, and sinuses (as well as certain reproductive anatomy in some AFAB patients). This is because the autoimmune response triggered by SS causes the body to produce less saliva, tears, and fluid in the aforementioned reproductive anatomy.
Unfortunately, these symptoms have a lot of comorbidity with other conditions, and so it’s very commonly misdiagnosed and underdiagnosed.
SS can also cause systemic issues. In my case, I often experience breathing difficulties at night caused by my dry sinuses (which are partially calcified) and the thickening of mucus in my throat. Additionally, I suffer from full body joint and nerve pain flares, fatigue flares, tooth decay (bacteria growth exacerbated by dry mouth), and brain fog and memory loss. SS can also potentially affect the function of vital organs and the gastrointestinal tract.
Unlike my Celiac disease, which can be controlled simply by eliminating gluten from my diet, my SS is managed with several medications that I must take daily (some throughout the day). I juggle a rheumatologist, an optometrist, a neuro-ophthalmologist, a dentist, an oral surgeon, and my primary care provider for the management of this disease. (On top of providers I see for other conditions.)
My Sjogren’s was diagnosed last year almost by happenstance in the course of trying to address pervasive double vision, which led to us discovering I had very dry eyes and an inflamed optic nerve, which led to me getting an MRI, which found a benign brain tumor, which led to me seeing a very knowledgeable neurologist who gave me a blood test for Sjogren’s related antibodies on a hunch and bam! I got my diagnosis and a referral to a rheumatologist. This is ironically a much more straightforward path to diagnosis than most SS patients experience and only took about three months.
(Sjogren’s had nothing to do with the double vision, which turned out to be muscular and fixable with prism glasses. Figuring out the inflamed optic nerve is ongoing.)
Both of these disorders are lifelong diagnoses, and there is currently no cure for either. Sjogren’s has the potential to progress to more severe symptoms with age. They are very exhausting to manage, and finding the right care team is critical.
Anyway, AMA!
What was your experience getting diagnosed with Celiac? Did you develop it as an adult?
And GF food and medications are expensive. Is there any financial support for your conditions?
And GF food and medications are expensive. Is there any financial support for your conditions?
Quote:
What was your experience getting diagnosed with Celiac? Did you develop it as an adult?
This one is long
I’ll answer these in reverse order, as it was a long, painful, and delayed road to getting my Celiac diagnosis. I can pinpoint symptoms of the disease going as far back as… five or six years old is when I remember the canker sores, tooth enamel issues, and stunted growth problems.
Celiac disease can manifest as early as when gluten is first introduced into a child’s diet, and it may not always manifest as gastrointestinal distress. I was very much an “eat bread out of the bag in front of the fridge” kid growing up, but I didn’t get sick after doing it. Celiac and gluten issues in general were far less understood back in the 90s and early 2000s than they are now, so we didn’t realize how many other things could be signs.
Celiac is a hereditary disease, meaning you are either born with the potential to develop it, or you’re not. In my case, both my paternal grandfather and a paternal great aunt have Celiac Disease.
The prevailing theory is that some sort of physical or emotional stress — such as a viral infection, surgery, or anxiety from a stressful life event — may "flip the switch" and cause the disease to appear in people who are genetically predisposed to it.
The majority of Celiac patients receive their diagnosis in adulthood, often at middle or advanced age. A lot of people only found out about their condition when nutritional deficiencies and symptoms such as extremely low bone density, etc. become a concern.
In my case, I started begging doctors for answers when I was in high school and developed stomach ulcers and GERD. At the age of 25, I was finally on my own insurance that covered specialists, so I saw my first gastroenterologist. Unfortunately, the correct order of events for diagnosing Celiac Disease is a bloodwork screening for specific antibodies, and then an endoscopy for confirmation. That was not my initial experience.
I was placed on an elimination/low FODMAP diet, which made me feel GREAT. But it had eliminated gluten from my diet without a blood test six weeks out from my scheduled endoscopy, so my body had time to heal. Thusly, no signs of Celiac were found.
I was referred to another gastro specialist in 2020 at 32 after not being able to keep food down without nausea meds for two months (my primary was Very Concerned). This one jumped right to the endoscopy, which to my shock confirmed Celiac Disease. He had me do the blood test after, and then I’ve been gluten-free ever since!
Celiac disease can manifest as early as when gluten is first introduced into a child’s diet, and it may not always manifest as gastrointestinal distress. I was very much an “eat bread out of the bag in front of the fridge” kid growing up, but I didn’t get sick after doing it. Celiac and gluten issues in general were far less understood back in the 90s and early 2000s than they are now, so we didn’t realize how many other things could be signs.
Celiac is a hereditary disease, meaning you are either born with the potential to develop it, or you’re not. In my case, both my paternal grandfather and a paternal great aunt have Celiac Disease.
The prevailing theory is that some sort of physical or emotional stress — such as a viral infection, surgery, or anxiety from a stressful life event — may "flip the switch" and cause the disease to appear in people who are genetically predisposed to it.
The majority of Celiac patients receive their diagnosis in adulthood, often at middle or advanced age. A lot of people only found out about their condition when nutritional deficiencies and symptoms such as extremely low bone density, etc. become a concern.
In my case, I started begging doctors for answers when I was in high school and developed stomach ulcers and GERD. At the age of 25, I was finally on my own insurance that covered specialists, so I saw my first gastroenterologist. Unfortunately, the correct order of events for diagnosing Celiac Disease is a bloodwork screening for specific antibodies, and then an endoscopy for confirmation. That was not my initial experience.
I was placed on an elimination/low FODMAP diet, which made me feel GREAT. But it had eliminated gluten from my diet without a blood test six weeks out from my scheduled endoscopy, so my body had time to heal. Thusly, no signs of Celiac were found.
I was referred to another gastro specialist in 2020 at 32 after not being able to keep food down without nausea meds for two months (my primary was Very Concerned). This one jumped right to the endoscopy, which to my shock confirmed Celiac Disease. He had me do the blood test after, and then I’ve been gluten-free ever since!
Quote:
And GF food and medications are expensive. Is there any financial support for your conditions?
This could wind up a broader commentary on the American social safety net or lack thereof, so I’ll try to keep it brief.
Because of my income level and disabilities (I receive federal benefits for my Bipolar and PTSD), I qualify for food stamps benefits (a monthly stipend that can be used for food - but not hot meals, it’s complicated). I get about $300, which covers two and a half grocery trips for me per month. I shop as lean as I can, and I go to Aldi to really make it stretch.
Another option for people with Celiac in the US is to save every receipt for a gluten-free alternative product, and then they can claim the difference in price between that and the regular product on their tax paperwork, which is INSANE and I never do it because it makes my ADHD brain cry.
Oof, what a drama getting diagnosed. And I it's really useful to know that you shouldn't cut gluten from your diet if you suspect you have celiac until you get tested!
Thank you so much for the answer!
Thank you so much for the answer!
What was the gluten free dish that surprised you with how freaking good it ended up being and that you can't seem to get enough of?
As another with Celiac Disease, I fully understand the struggles that come with it. How sensitive to gluten are you?
Can you touch things with gluten in it?
Does corn bother you too? (It hates me)
Do heavily processed ingredients derived from wheat or barley still hurt?
Do you have to resort to grass fed meat and dairy instead of the standard grain fed cause it angers your body?
Sorry for the bombardment.
Can you touch things with gluten in it?
Does corn bother you too? (It hates me)
Do heavily processed ingredients derived from wheat or barley still hurt?
Do you have to resort to grass fed meat and dairy instead of the standard grain fed cause it angers your body?
Sorry for the bombardment.
Sanne wrote:
What was the gluten free dish that surprised you with how freaking good it ended up being and that you can't seem to get enough of?
I was never hugely into Thai before my Celiac diagnosis, but since then, the Thai place here in town is one of a couple of safe places to eat at/order from. I love the Siam fried rice (honestly the best fried rice I've ever had) and this dish called Pad See You which is a stir fry with the wide, flat rice noodles. I love to load them up with extra veggies and an extra egg. Suuuuper filling and tasty!
I was ordering so much at one point that they knew my usual order and held the scallions and cilantro in the soup I liked when I forgot to request it one time. Chef Roy is the real MVP. ;o;
LunarValravn wrote:
As another with Celiac Disease, I fully understand the struggles that come with it. How sensitive to gluten are you?
Can you touch things with gluten in it?
Can you touch things with gluten in it?
I have become significantly more sensitive since I went totally gluten-free, however prior to my diagnosis, I would rarely have obvious symptoms when I consumed gluten except beer. I just kind of assumed that everyone felt bloated and terrible after drinking beer for YEARS. Now I can't eat anything that's touched the same surface as gluten without feeling like my stomach is trying to claw its way out of my esophagus. I have been cross contaminated three times in four years, and WHEW it was a bad time. It's like seasonal allergies plus bloating plus horrible pain.
I am able to touch things with gluten, however I wash my hands immediately after and am careful not to touch my mouth/face. This is rarely a concern, though, as I live alone and have a dedicated gluten-free kitchen, and, well... I don't get out much. When I am at others' houses, I'm not the one doing the cooking or food handling, usually.
Quote:
Does corn bother you too? (It hates me)
I have MANY intolerances, but I mercifully seem to tolerate corn just fine. I would cry if I couldn't because it's one of my favorite foods. I have to label watch even certified gluten-free foods like a hawk though because chickpeas are in so many of them, and I'm severely intolerant. I need corn and rice to survive. ;o;
Quote:
Do heavily processed ingredients derived from wheat or barley still hurt?
I honestly don't know. Like I said above, I have a dedicated gf kitchen, and for financial and non-Celiac related health reasons, I do not eat many heavily processed foods. I mostly cook from scratch with safe ingredients.
Quote:
Do you have to resort to grass fed meat and dairy instead of the standard grain fed cause it angers your body?
Thankfully I can tolerate grain fed meat safely. I've never had an adverse reaction to any meat that I've consumed, which is good because my diet is basically meat, some fruit, and vegetables for the most part. Meat has been one of my only totally safe things I can eat since I went low FODMAP in 2012.
It's much the same for dairy. I have a lactose intolerance, but I've never had a reaction to Lactaid (or the Aldi equivalent).
You are on: Forums » Smalltalk » AMA: Living with Celiac & Sjogren's Syndrome